Abbreviations:
anterior sphenoid sinus wall
;
INTRODUCTION
Due to the potential for serious consequences, complications involving the optic nerve are always a concern in transnasal endoscopic surgery, particularly when the orbit, the posterior paranasal sinuses, the optic canal (OC), or the skull base are involved. Patients who are at an increased risk for these complications include those with extensive disease, those undergoing revision surgery, those with anatomical variations due to previous disease or surgery, and those who have been exposed to the use of powered instrumentation. Preventing these complications relies on a thorough understanding of anatomy, adequate preparation, the ability to foresee potential problems, and experience [
1-
3].
Studies conducted on this topic have highlighted the importance of understanding the anatomy of the orbital apex, given its proximity to vital anatomical structures within a confined space. Numerous variations in the anatomy of the orbital apex and its adjacent structures, such as the orbits, the posterior paranasal sinuses, the OC, and the skull base, have been discussed in the literature. However, the extensive range of anatomical variations in this complex region calls for additional research. This will not only enhance our understanding but also have significant clinical implications for planning and performing surgery [
4-
6].
In this study, we investigated the bone landmarks within the orbital apex and associated areas. These included the optic foramen (OTF), the opening of the OC, the anterior sphenoid sinus wall (ASW) where it connects to the medial orbital wall (MOW), and the carotid prominence (CP) located in the posterior sphenoid sinus. Understanding the correlations and variations among these landmarks could provide valuable guidance for surgeons performing endoscopic transnasal surgery in the orbital apex and surrounding regions.
METHODS
This retrospective study included participants who underwent computed tomography (CT) scans of their orbits and sinuses at a tertiary hospital in Ho Chi Minh City, Vietnam, between December 2022 and March 2023. The study was approved by the institutional review board/ethics committee. All research procedures were conducted in accordance with the principles of the Declaration of Helsinki.
The inclusion criteria for this study were patients aged 18 years or older, with normal CT scans of their orbits and sinuses, irrespective of the reasons for the scans. Patients who had any notable abnormalities in their orbits or sinuses as seen on CT scans, or those who had a history of orbital or sinus surgery, were not included in the study.
A Siemens 64 multi-slice CT scanner was used to collect images with a bone-window, multiple planes (axial, coronal, and sagittal) and thin axial slices ( < 0.8 mm). A single radiologist, who was certified in craniofacial pathology, reviewed all CT images and performed all measurements as described below.
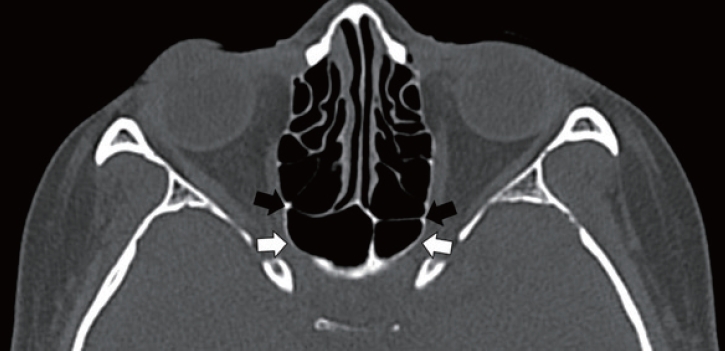
The locations of the medial end of the OTF, the superolateral aspect of the ASW where it merges with the MOW, and the CP in the posterior sphenoid sinus were determined by simultaneously examining the participant’s CT slices in all three planes: axial, coronal, and sagittal. The position of the OTF was identified as either anterior or posterior to the ASW. If the OTF’s position was the same in both the right and left orbit, it was deemed symmetrical. Conversely, if the location differed in each orbit, it was deemed asymmetrical (
Figs. 1-
3). The distances from the OTF to the ASW, as well as the distances from both the OTF and ASW to the CP, were measured using a digital caliper in thin axial slices and in a front-to-back direction (mm) (
Fig. 4). These landmarks, correlations, and measurements are consistent with previously published studies [
4,
5,
7].
To ensure accuracy and consistency, the entered data were cross-checked to verify that all variables were properly filled out before analysis. Stata version 14 (StataCorp.) was used for the statistical analysis. The Shapiro-Wilk test confirmed the normal distribution of the data; hence, mean results are reported throughout this article. A two-tailed paired t-test analysis was performed to explore potential discrepancies between the right and left orbits. A simple regression analysis was conducted to investigate the correlation between all measurements and variables (laterality, sex, and age) incorporated in the study. A p-value of less than 0.05 was used to determine statistical significance.
RESULTS
The study included 200 orbits from 100 participants, consisting of 55 females (55%) and 45 males (45%). The participants’ ages varied from 18 to 85 years, with an average age of 41.13 ± 13.75 years. All CT scans were deemed normal, irrespective of the reasons for conducting the scan. None of the patients had a history of sinus or orbital surgery, nor did they have any significant abnormalities in the sinus or orbital region.
In women, the OTF was located anterior to the ASW in 49.1% of the orbits, with the remaining 50.9% having the OTF positioned posteriorly. In men, the respective percentages were 47.8% anterior and 52.2% posterior. When considering both sexes, the OTF was found to be anterior to the ASW in 48.5% of orbits, while it was posterior in the remaining 51.5%. In women, the OTF was found to be symmetrical on both sides in 63.64% of the orbits, while the remaining 36.36% exhibited asymmetry. In men, symmetry was observed in 66.67% of the orbits, with the remaining 33.33% showing asymmetry. When both sexes were evaluated, the OTF was symmetrical on both sides in 65% of the orbits, and asymmetrical in the remaining 35%. The results of all measurements, including the mean distance from the OTF to the ASW, the mean distance from the OTF to the CP, and the mean distance from the ASW to the CP are summarized in
Table 1. No statistically significant correlations were found in our data between any of the measurements and variables, including age, sex, and the side of the orbit.
DISCUSSION
The findings of our study underscore the significance of identifying the location, the correlation and the distance between the OTF, the ASW and the CP. A clear understanding of these variations can be beneficial for surgeons in planning and performance endoscopic transnasal surgery.
Our study revealed that the OTF was located anterior to the ASW in 51.5% of the orbits, while it was posterior in the remaining 48.5%. The findings of our study closely match those reported by Cinaroglu et al. [
4] and Aujla et al. [
5], showing that the OTF was located anterior to the ASW in 46% and 50% of the orbits, respectively. The slight discrepancies could potentially be due to variations in the race and sex of the participants.
The correlation between the OTF and the ASW provides crucial data for surgeons, enabling them to examine the relationship between the OC and the posterior paranasal sinuses [
5,
8]. The OTF is the entrance to the OC, running along the lateral side of the posterior paranasal sinuses. If the OTF is positioned anterior to the ASW, it means that the OC also begins anterior to the ASW. Our research showed that in approximately half of the orbits studied, the OTF was situated anterior to the ASW. This suggests that the OC also began anterior to the ASW in roughly half of the cases examined. In such scenarios, surgery involving either the posterior ethmoid sinus or the ASW could potentially lead to direct OC injury. Therefore, it is imperative for surgeons to be aware of the OTF and OC locations to reduce the risk of optic nerve complications during endoscopic sinus surgery related to the posterior paranasal sinus, including both the ethmoid and sphenoid sinuses.
Understanding the relationship between the OTF and the ASW can provide valuable assistance to surgeons in planning and performing surgery for sinonasal tumors involving the MOW and the ASW. Tumors in the sinonasal region have the potential to extend along the MOW and enter the orbit, the OC, and the sphenoid sinus. If a CT scan shows signs of tumor expansion from the MOW to the ASW, and the OTF is located anterior to the ASW, the tumor can involve the OC and the optic nerve within the OC. In such cases, it is crucial to carefully scrutinize magnetic resonance imaging for signs of optic nerve invasion [
9].
The correlation between the OTF and the ASW may influence the surgical approach in orbital decompression surgery. To achieve optimal orbital decompression, surgeons may need to perform a MOW opening that extends up to the orbital apex, including the OTF. If the OTF is located posterior to the ASW, the surgeon may have to enter the sphenoid sinus and remove a part of its anterior-lateral wall to achieve complete decompression. In such cases, the endoscopic trans-sphenoidal technique may be a more suitable approach [
5]. Therefore, the location of OTF relative to the ASW is essential in deciding between the endoscopic trans-sphenoidal technique and other techniques for certain patients [
5,
10,
11]. In our study, the OTF was positioned posterior to the ASW in 48.5% of the orbits. This suggests that in nearly half of the cases we examined, accessing the sphenoid sinus would be necessary to achieve full orbital decompression when required. Other anatomical factors, such as the angle of the ASW where it merges with the MOW, may also influence the need to access the sphenoid sinus and the pneumatization of the sphenoid sinus [
5,
12]. While these parameters are beyond the scope of our study and we do not speculate on them, it is important to highlight the significance of these anatomical variations during surgical procedures. Further research is needed to fully understand these factors.
In our study, 65% of cases showed a symmetrical OTF location between the left and right orbit within the same individuals. However, the remaining 35% displayed asymmetry. These insights could be beneficial for surgeons during revision surgery, where previous procedures may have altered anatomical landmarks, or in instances where the disease has impacted one side.
The close proximity of key landmarks, including the OC, CP, and skull base, makes surgical procedures entering the sphenoid sinus potentially riskier [
13]. In our study, the mean distance from the OTF to the ASW, the mean distance from the OTF to the CP and the mean distance from ASW to the CP were 3.82 ± 1.25 mm, 7.67 ± 1.73 mm, and 7.95 ± 2.53 mm, respectively. While the measurements obtained in our study were slightly lower than those reported by Aujla et al. [
5] and Cinaroglu et al. [
4], the range of parameters we found falls well within the range of variation described by those authors. Surgeons performing procedures in this area should be acquainted with the relationship between the OTF, the ASW and the carotid artery.
One notable drawback of this study is that conventional CT scans may not offer a comprehensive view of the essential landmarks discussed herein. To obtain optimal views, it may be necessary to reconstruct the images and tilt the CT slice plane during the pre-surgery planning phase. During surgery, the use of an image-guided system may help in identifying these landmarks when necessary, thereby reducing the risk of optic nerve injury [
14,
15].