INTRODUCTION
Parotid sialocele refers to the accumulation of saliva in tissues around the parotid gland duct or parenchyma caused by insufficient excretion of saliva. Trauma-related duct damage is the most common cause of this condition, and other causes include infection, neoplasm, duct stenosis, and iatrogenic causes following parotid surgery [
1,
2]. Parotid sialocele is diagnosed based on the patient’s history and clinical evaluation. Imaging helps determine the size of the injury, location, and treatment method. Inappropriate sialocele treatment can result in an external fistula, facial asymmetry, or secondary infection [
3,
4]. An anastomosis or ductal reconstruction should be performed within 24 hours of parotid duct injury. Delayed treatment remains a matter of debate, and the choice of treatment depends on whether the goal is to preserve or suppress gland function. Conservative protocols for suppressing gland function are widely used, including periodic percutaneous aspiration, pressure dressing, botulinum toxin, and antisialogogue agents [
5,
6]. In particular, the use of antisialogogue agents can help inhibit salivary secretion and alleviate autolysis of soft tissues, which could lead to delayed wound healing or infection [
7]. Furthermore, transdermal scopolamine—an antisialogogue agent—has been widely used in recent years due to its minimal side effects and convenient administration method [
8]. We aimed to present the successful treatment of recurrent sialocele with a transdermal scopolamine patch.
CASE REPORT
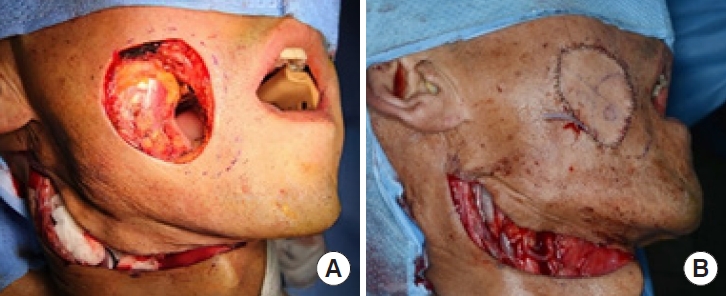
A 65-year-old man with a history of hypertension, diabetes mellitus, and hepatitis presented with a painful mass on his right buccal region. A punch biopsy of the right buccal mucosa, performed by the otorhinolaryngology department, revealed squamous cell carcinoma of the right buccal mucosa. Preoperative positron emission tomography-computed tomography showed no evidence of distant metastasis. Wide excision of the right buccal mucosa was performed, including the overlying skin. This resulted in a skin defect on the right cheek. Next, right supraomohyoid neck dissection was carried out, followed by reconstruction with a folded free anterolateral thigh flap. The proximal and distal portions of the thigh flap were designed according to the defect size, and the intervening area was de-epithelialized after flap elevation. Subsequently, the flap was folded to create the intraoral mucosal lining and cover the facial side of the cheek (
Fig. 1). During mass removal, a segment of the parotid duct was excised, and ductal ligation was then performed to prevent sialocele occurrence. The final pathology report confirmed a 1.7 × 0.9 cm squamous cell carcinoma with a maximum invasion depth of 0.6 cm, consistent with the punch biopsy results. No evidence of lymph node metastasis was observed, and the patient was diagnosed with stage T2N0M0 disease.
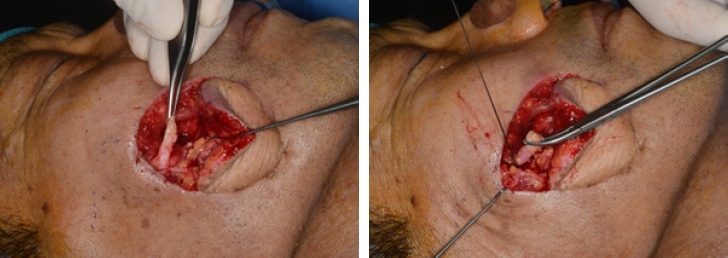
At 22 days after surgery, clear, saliva-like drainage was observed, and neck computed tomography revealed a 25.73-mm-diameter fluid collection with air density (
Fig. 2). Ligation of the right salivary duct (Stenson’s duct) was planned under local anesthesia through the external approach. The ligation was performed at the proximal site first, and to prevent any loosening, the distal end was bent and then subjected to another ligation along with the proximal site (
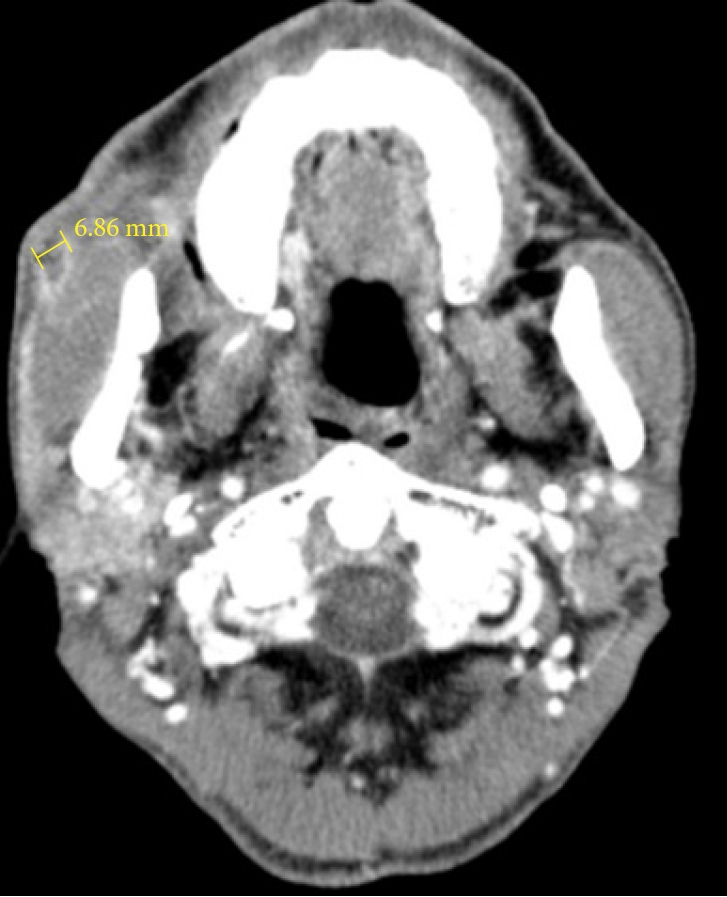
Fig. 3). The swelling subsided after ligation, and the patient was discharged. However, 21 days post-ligation, swelling and clear drainage recurred at the surgical site. Neck computed tomography showed a decrease in the extent of fluid collection. The fluid collection was located at the right anterior aspect of the masseter muscle and was proximal to the ligation. Its long-axis diameter was 6.86 mm (
Fig. 4). The patient was prescribed antibiotics for 2 weeks, and a pressure dressing was applied. Nonetheless, leakage persisted, and the patient was treated with antibiotics and a pressure dressing along with the application of a transdermal scopolamine patch (1.5 mg) for 3 weeks, with one patch applied every 3 days [
9]. By this time, the swelling had subsided, and it did not recur.
DISCUSSION
Due to the complex anatomy of the face, tumor removal and subsequent reconstruction pose significant challenges. In particular, the parotid gland, which lies superficially just behind the masseter muscle, is often at risk of injury during facial surgery. The parotid duct, which is approximately 7 cm long, originates from the anterior part of the parotid gland, and passes along the anterior surface of the masseter. It runs alongside the transverse facial artery and the buccal branch of the facial nerve and then penetrates the buccinator muscle and oral mucosa [
5,
10,
11].
Parotid gland and duct injuries are typically identified a few days after surgery. Surgical interventions, such as proximal duct ligation, parasympathetic denervation, and internal fistula creation to redirect salivary flow into the oral cavity, can be helpful [
12]. In the present case, ductal ligation was performed during mass removal; however, despite ductal ligation, sialocele occurred. Furthermore, the sialocele recurred despite performing a second rigid ligation. Sialocele may recur due to pressure from saliva discharge in the parotid duct, causing leakage. Ultimately, suppressing the parotid gland until proper wound healing is achieved is essential.
Antisialogogues, including scopolamine, are commonly used conservative treatments for suppressing parotid gland function, but systemic antisialogogues can have many potential side effects, such as dry mouth, constipation, photophobia, tachycardia, and urinary retention [
13]. Additionally, the use of intravenous, intramuscular, or subcutaneous scopolamine requires three injections per day, which may cause patient discomfort.
Transdermal scopolamine patches, which were first developed for preventing motion sickness, are widely used for various purposes. As a muscarinic receptor antagonist, scopolamine reduces daily salivary output. A transdermal scopolamine patch applied to the hairless skin behind the ear ensures a consistent rate of absorption, maintaining a stable plasma level for at least 72 hours. It has minimal side effects and is a noninvasive method that the patient can easily apply and remove. In this case, one transdermal scopolamine patch, containing 1.5 mg of scopolamine, was applied every 3 days on the postauricular area and achieved the resolution of sialocele.
In conclusion, parotid sialocele is a rare condition that may occur after surgery, particularly if the operation involves structures around the parotid gland. Although surgical intervention remains the first-line treatment, transdermal scopolamine can also be a useful adjunctive treatment for recurrent parotid sialocele. Furthermore, if injury to the parotid gland or duct is anticipated, the prophylactic use of a transdermal scopolamine patch until proper wound healing occurs can be a good therapeutic option to prevent sialocele.